- About Us
- Meet the Team
- Locations
-
Patient Resources
-
-
Patient Information
-
Patient Information
-
-
- Services
Proudly Part of Privia Health
Diabetic Retinopathy watching out
Patients with diabetes are at risk for damage to multiple areas of the eye, including:
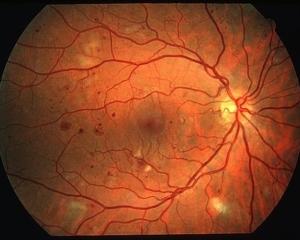
- Retina - The most common cause of vision loss among patients with diabetes, diabetic retinopathy affects the part of the eye that is sensitive to light.
- Macula - When diabetic retinopathy is present, there can be swelling and damage of the macula, the area of the eye responsible for sharp, central vision. The risk for macular edema increases as diabetic retinopathy progresses. About half of diabetic patients with retinopathy will develop macular edema, making it the most common cause of vision loss among people with diabetic retinopathy.
- Lens - cataracts (clouding of the lens of the eye) are more common and tend to occur earlier in life in patients with diabetes
- Optic nerve - Glaucoma, elevated eye pressure, causes damage to the optic nerve (the information highway between the eyes and the brain). Diabetes doubles a person's risk for glaucoma.
Let's focus on retinopathy
The retina is the part of the eye that detects light and converts it to signals that are sent through the optic nerve, to the brain. Chronically high blood sugar causes damage to the tiny blood vessels of the retina, resulting in the leaking of fluid, bleeding or ischemia (poor blood supply). This results in distortion of vision. If the damage progresses, new abnormal blood vessels form, grow and bleed, leading to irreversible scarring and obliteration of the retina.
Diabetic retinopathy is defined by four stages:
- Mild nonproliferative retinopathy -- small balloon-like swellings form in the tiny blood vessels of the retina (microaneurysms). These microaneurysms can leak fluid or bleed into the retina.
- Moderate nonproliferative retinopathy -- blood vessels feeding the retina become swollen and distorted, sometimes loosing their ability to transport blood. The macula, responsible for sharp, central vision can be affected at this stage.
- Severe nonproliferative retinopathy -- continued blood vessel swelling and distortion, leading to significant deprivation of nourishment and oxygen to areas of the retina. These deprived areas secrete growth factors to promote new blood vessel growth.
- Proliferative retinopathy -- Unfortunately, the new blood vessels that are formed in the retina are like weeds in a garden. They grow along the inside surface of the retina and invade the vitreous gel that fills the eye. In addition, they are fragile and tend to bleed, resulting in scar formation. This scar tissue can contract, pulling the retina away from the underlying tissue and causing retinal detachment and permanent vision loss.
What can you do? Take care of yourself.
- Keep your blood sugar under control -- patients who keep their blood glucose as close to normal as possible are significantly less likely to develop retinopathy (as well as all the other complications of diabetes)
- Keep your cholesterol under control -- patients with elevated cholesterol have increased risk for vision loss
- Get screened for diabetic retinopathy
What can we do? Screen your eyes for diabetic retinopathy.
Finally, some good news! Screening for diabetic retinopathy can be done during a routine visit to our office. After a few minutes of sitting in a darkened room (to naturally dilate your pupils), we will take a picture of your retina with a special camera. (Infrequently eye drops are needed to help dilate the pupils.) The picture is informally read by Dr. Banarer and then sent electronically to an opthamologist who formally reads the picture for signs of diabetic retinopathy. This includes looking for:
- Changes to blood vessels
- Leaking blood vessels or warning signs of leaky blood vessels, such as fatty deposits
- Swelling of the macula (diabetic macular edema)
- Changes in the lens
- Damage to nerve tissue
We receive a report from the opthamologist within 24 hours and then share the report with you.
Who should be screened for diabetic retinopathy?
Everyone with diabetes is at risk for diabetic retinopathy, and the longer a person has had diabetes, the higher their risk. Unfortunately, even women with only gestational diabetes (diabetes during pregnancy) are at risk. There are usually no symptoms of vision impairment in the early stages of retinopathy -- almost half of Americans with diabetes have some stage of diabetic retinopathy, but only half of them are aware of it.
Everyone with diabetes should have an initial screening exam for retinopathy. In a person with good health, retinopathy exams can be performed at 1-2 year intervals. If retinopathy is present, eye exams are done more frequently.
How does screening help?
Blindness due to late-stage retinopathy is permanent. But, early detection and treatment of retinopathy can markedly reduce the risk of vision loss. There are a variety of treatment options available.. stay tuned for a future post!